Table of Contents
Introduction
Type 2 Diabetes is more than a diagnosis—it’s a lifelong journey requiring continuous care. For clinicians, finding the balance between evidence-based strategies and individualized patient care is the key to optimizing outcomes. So, what practical steps can healthcare providers take to help their patients thrive? Let’s explore cutting-edge approaches and proven tactics that are reshaping diabetes care.
Understanding Type 2 Diabetes
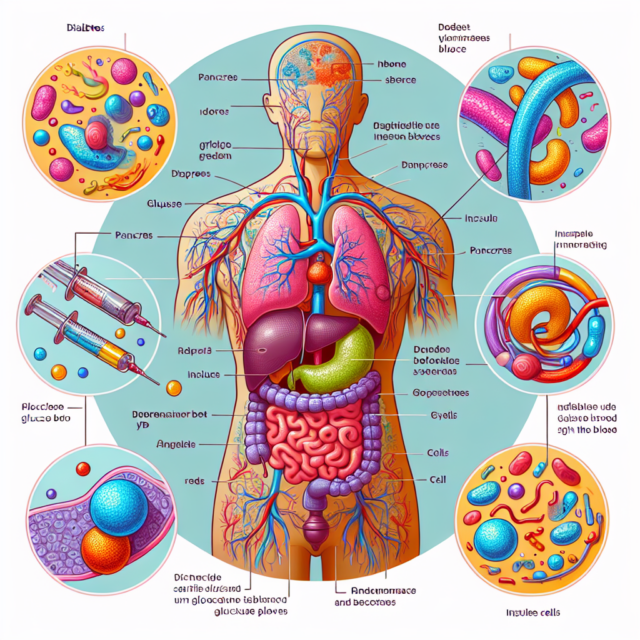
Type 2 Diabetes is a chronic condition where the body becomes resistant to insulin or doesn’t produce enough of it. This imbalance leads to elevated blood sugar levels, impacting everything from cardiovascular health to wound healing. Understanding the disease’s systemic impact is essential for creating comprehensive care plans.
The Importance of Early Diagnosis
Did you know early diagnosis can delay complications by years? Screening tools like HbA1c tests and fasting glucose levels are crucial. Identifying prediabetes in at-risk populations can enable interventions that prevent progression to full-blown Type 2 Diabetes.
Personalized Treatment Plans
No two patients are the same, and their diabetes care shouldn’t be either. Individualized treatment plans should consider factors like age, comorbidities, and patient preferences. Tailoring approaches leads to better adherence and improved outcomes.
Leveraging Lifestyle Interventions
Lifestyle changes are often the cornerstone of Type 2 Diabetes management. Encouraging regular exercise and a balanced diet rich in whole grains, lean proteins, and vegetables can significantly lower HbA1c levels. A great analogy is viewing lifestyle interventions as the “foundation” of a diabetes care house—everything else builds on it.
Medication Management
Medications like metformin remain the gold standard, but newer agents such as SGLT2 inhibitors (e.g., Jardiance) and GLP-1 receptor agonists (e.g., Ozempic) offer additional benefits, including weight loss and cardiovascular protection. Understanding drug mechanisms helps clinicians fine-tune therapy to patient needs.
Monitoring and Managing Comorbidities
Managing Type 2 Diabetes often means addressing the broader health picture. Conditions like hypertension, dyslipidemia, and obesity frequently accompany diabetes. Regular screenings for diabetic retinopathy, neuropathy, and nephropathy ensure complications are caught early and managed effectively.
Harnessing Technology in Diabetes Care
Technology is transforming diabetes management. Tools like continuous glucose monitors (CGMs) provide real-time insights, while telehealth platforms enhance accessibility. Even apps that track nutrition and activity levels can empower patients to take control of their health.
Engaging Patients for Long-Term Success
A successful diabetes care plan involves more than just prescriptions—it requires patient buy-in. Motivational interviewing and shared decision-making strengthen the clinician-patient relationship. Educational resources, like those on Diabetes in Control, can help bridge knowledge gaps.
Preventing Complications
Complications such as cardiovascular disease and diabetic foot ulcers can drastically reduce quality of life. Proactive measures, including regular check-ups, smoking cessation programs, and routine foot care, are non-negotiable.
Innovative Research and Future Trends
Emerging therapies like beta-cell regeneration and artificial pancreas systems offer hope for the future. Keeping abreast of clinical trials and advancements ensures patients benefit from the latest innovations.
Conclusion
Optimizing Type 2 Diabetes management is a dynamic process requiring a blend of science, empathy, and innovation. By focusing on early diagnosis, personalized care, and patient engagement, clinicians can help individuals live fuller, healthier lives despite their diagnosis.
FAQs
1. What is the most effective first-line treatment for Type 2 Diabetes?
Metformin is widely regarded as the first-line treatment due to its efficacy, safety profile, and cost-effectiveness.
2. How can technology improve diabetes management?
Technologies like CGMs and telehealth improve monitoring, enhance communication, and provide actionable data for better decision-making.
3. Are SGLT2 inhibitors safe for all patients?
While highly effective, SGLT2 inhibitors may not suit patients with kidney disease or recurrent urinary tract infections.
4. How can clinicians encourage lifestyle changes in patients?
Motivational interviewing, goal setting, and patient education are proven ways to foster lasting lifestyle changes.
5. What is the role of GLP-1 receptor agonists in diabetes care?
These medications help regulate blood sugar, aid weight loss, and reduce cardiovascular risks, making them an excellent option for many patients.