Introduction
Managing diabetes often feels like steering a ship through stormy waters. Clinicians know that blood sugar control is the central compass guiding patient care. But what truly matters most when treating patients with diabetes? Is it medication, lifestyle modification, or something deeper? This article explores critical strategies that healthcare providers must prioritize to achieve optimal outcomes.
Table of Contents
- Understanding the Fundamentals of Blood Sugar Control
- Pharmacological Advances and Branded Drug Options
- Lifestyle Interventions: The Cornerstone of Care
- Monitoring, Technology, and Patient Empowerment
- Conclusion
- FAQs
Understanding the Fundamentals of Blood Sugar Control
Every healthcare provider managing diabetes must first appreciate the significance of blood sugar control in reducing complications such as neuropathy, retinopathy, and cardiovascular disease. Glycemic control isn’t just about hitting target numbers; it’s about comprehensive, individualized management.
The American Diabetes Association (ADA) recommends an HbA1c target of <7% for most adults with diabetes. However, individualized targets are crucial based on age, comorbidities, and risk factors. Transition words such as “moreover,” “thus,” and “consequently” play a pivotal role in explaining these nuanced care strategies.
In addition to HbA1c, postprandial glucose levels and time-in-range (TIR) metrics have gained attention. TIR, the percentage of time a patient spends within target glucose ranges, correlates closely with reduced microvascular complications. According to a 2023 study in “Diabetes Care,” maintaining a TIR above 70% significantly lowers the risk of adverse outcomes.
Pharmacological Advances and Branded Drug Options
Pharmacotherapy has dramatically evolved in diabetes management. New drug classes are reshaping the blood sugar control landscape.
SGLT2 Inhibitors like Jardiance (empagliflozin) and Farxiga (dapagliflozin) not only lower glucose but also provide cardiovascular and renal benefits. For many patients, these agents have shifted the therapeutic goalposts.
Meanwhile, GLP-1 receptor agonists such as Ozempic (semaglutide) and Trulicity (dulaglutide) offer dual advantages of glucose lowering and weight loss. Healthcare professionals must be aware that these drugs may improve patient adherence and satisfaction significantly.
When initiating insulin therapy, new basal insulin analogs like Toujeo (insulin glargine U-300) offer more stable profiles, reducing nocturnal hypoglycemia risk. Combining multiple agents often enhances blood sugar control but must be balanced against potential side effects.
Notably, Diabetes in Control regularly publishes updates on novel pharmacotherapies, providing a rich internal resource for staying informed.
Lifestyle Interventions: The Cornerstone of Care
Medications alone cannot achieve comprehensive blood sugar control. Thus, lifestyle interventions remain the foundation.
Nutrition Therapy is critical. Encouraging patients to adopt a Mediterranean diet or plant-based eating patterns leads to better glycemic control and overall health. Importantly, collaboration with dietitians ensures patients receive practical, sustainable advice.
Physical Activity amplifies insulin sensitivity. Moderate-intensity exercise—like brisk walking—for at least 150 minutes weekly remains the gold standard. However, recommending tailored exercise plans is vital, particularly for patients with cardiovascular or orthopedic limitations.
Weight Management also plays an integral role. Even a modest weight loss of 5-7% significantly improves blood sugar control. Semaglutide, in higher doses (Wegovy), has been a game-changer for weight loss interventions among patients with type 2 diabetes.
Patient-centric strategies—motivational interviewing, setting SMART goals, and tracking progress—improve engagement and outcomes. Clinicians can direct patients to forums like HealingWell’s diabetes forum for peer support and community discussions.
Monitoring, Technology, and Patient Empowerment
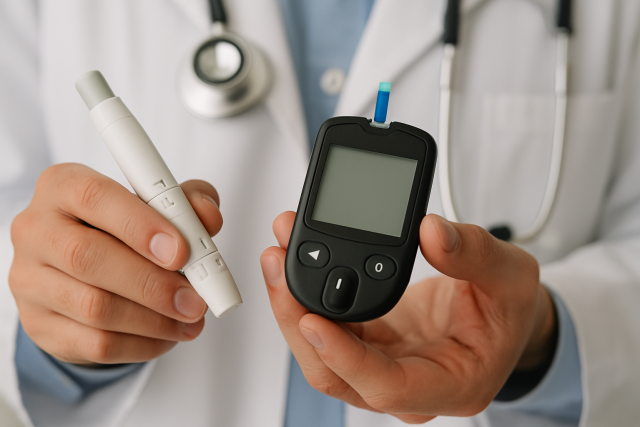
Gone are the days when a quarterly HbA1c was the sole measure of success. Continuous glucose monitoring (CGM) systems like Dexcom G7 and Abbott’s FreeStyle Libre 3 are revolutionizing blood sugar control.
CGMs provide real-time data, helping clinicians and patients identify glycemic patterns, anticipate lows and highs, and adjust therapy dynamically. According to recent research in “The Lancet Diabetes & Endocrinology,” CGM users saw a 0.5% greater reduction in HbA1c compared to traditional self-monitoring of blood glucose.
Moreover, apps that sync CGM data to smartphones facilitate remote monitoring and telehealth interventions. Empowered patients who understand their glucose patterns are more likely to engage in proactive health behaviors.
Education remains essential. Providers should dedicate time to teaching patients about CGM interpretation, medication titration, and lifestyle adjustments. Free patient resources from Diabetes in Control can support structured education programs.
Conclusion
In the complex journey of managing diabetes, blood sugar control remains the beacon that guides healthcare providers. Pharmacological innovations, lifestyle interventions, patient education, and technology integration collectively enhance outcomes.
However, successful management ultimately hinges on personalized, compassionate care. By leveraging all available tools—from branded medications like Jardiance and Ozempic to CGMs and community resources—clinicians can dramatically improve their patients’ quality of life.
FAQs
What is the optimal HbA1c target for most adults with diabetes?
Most adults should aim for an HbA1c of less than 7%, although targets should be individualized.
Which branded drugs help with both blood sugar control and weight loss?
GLP-1 receptor agonists like Ozempic and Trulicity aid both glycemic control and weight management.
How often should continuous glucose monitoring be recommended?
CGM can benefit patients with frequent hypoglycemia, intensive insulin regimens, or those struggling with blood sugar variability.
Can lifestyle changes alone manage type 2 diabetes?
In early stages, lifestyle changes may suffice, but pharmacologic interventions are often needed as the disease progresses.
Where can patients find supportive diabetes communities online?
Patients can join forums like HealingWell for peer support and practical advice.
This content is not medical advice. For any health issues, always consult a healthcare professional. In an emergency, call 911 or your local emergency services