Living with diabetes is already a challenging journey, but what happens when you add stroke risk into the mix? Think of your blood vessels as highways; when blood sugar runs high, it’s like a constant traffic jam that wears down the roads. Eventually, that wear and tear can trigger a diabetic stroke—a serious, life-threatening event.
Understanding the connection between diabetes and stroke is critical for both prevention and early treatment. This article explores how likely a diabetic stroke is, the signs to watch for, and what steps can help you reduce your risk.
Table of Contents
- What Is a Diabetic Stroke?
- Why Does Diabetes Increase Stroke Risk?
- Key Warning Signs and Symptoms
- How to Prevent a Diabetic Stroke
- Conclusion
- FAQs
What Is a Diabetic Stroke?
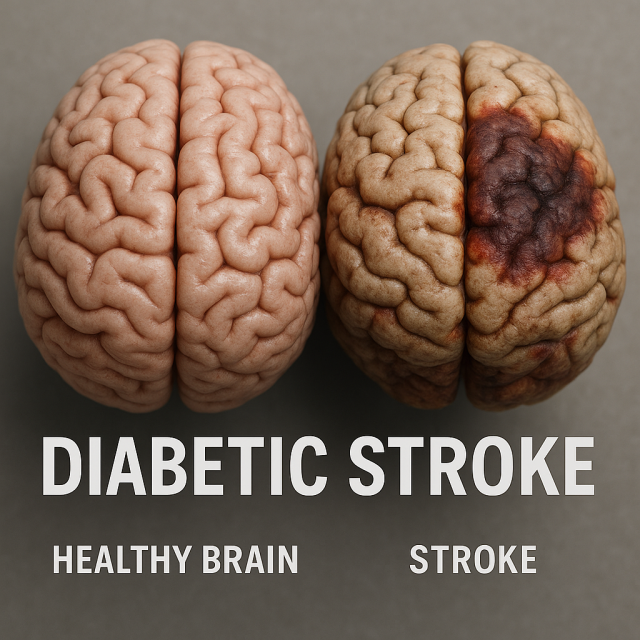
A diabetic stroke occurs when reduced blood flow to the brain is caused or worsened by diabetes-related damage. Like any stroke, it can lead to brain injury, long-term disability, or death. However, people with diabetes face a significantly higher risk compared to those without the condition.
According to the American Diabetes Association, individuals with diabetes are 1.5 times more likely to experience a stroke. This risk increases if blood sugar is poorly managed or if other conditions such as high blood pressure or high cholesterol are present.
In type 2 diabetes, the risk is compounded by insulin resistance, obesity, and chronic inflammation, all of which impact blood vessels and circulation. The longer a person has diabetes, the higher the chances of vascular complications—including stroke.
In fact, stroke is one of the top complications associated with diabetes, often overlapping with heart disease, neuropathy, and kidney problems.
Why Does Diabetes Increase Stroke Risk?
The link between diabetes and stroke is not just correlation—it’s causation. Elevated glucose levels over time damage blood vessels and nerves that control the heart and brain. This process, called atherosclerosis, thickens artery walls and increases clot formation, setting the stage for both ischemic and hemorrhagic strokes.
Here’s how the pieces come together:
- High blood sugar: Consistently elevated glucose leads to vessel inflammation and plaque buildup.
- Hypertension: Over 70% of adults with diabetes also have high blood pressure, a leading stroke trigger.
- Dyslipidemia: Diabetics often have abnormal cholesterol levels—high LDL and triglycerides, low HDL.
- Obesity and inactivity: Common in type 2 diabetes, these factors exacerbate cardiovascular strain.
- Insulin resistance: A key player in metabolic syndrome, increasing the likelihood of clotting events.
In some cases, certain medications or lifestyle habits (such as smoking or alcohol use) may further elevate stroke risk. Even some branded drugs used for glucose control must be monitored carefully for cardiovascular impact.
The American Heart Association has stressed that **managing ABCs—A1C, Blood Pressure, and Cholesterol—**is essential for lowering stroke risk in diabetes patients. Newer medications like Jardiance, Farxiga, and Ozempic have shown promising cardiovascular benefits when used appropriately.
Key Warning Signs and Symptoms
Stroke symptoms tend to appear suddenly, but knowing them in advance can save your life. Diabetics must remain extra vigilant, as symptoms can sometimes be masked or misinterpreted due to diabetic neuropathy or poor blood sugar control.
Common warning signs include:
- Sudden numbness or weakness, especially on one side of the body
- Confusion, trouble speaking, or difficulty understanding speech
- Sudden trouble seeing in one or both eyes
- Dizziness, loss of balance, or difficulty walking
- Sudden severe headache with no known cause
If you or someone else experiences these symptoms, call 911 immediately. Early intervention—often within the first three hours—can dramatically improve outcomes.
Additionally, symptoms like blurred vision or numb limbs can mimic low or high blood sugar episodes, which means diabetics must learn to distinguish between hypoglycemia and a stroke. When in doubt, it’s better to err on the side of caution.
For more clinical details on symptom management and glycemic complications, visit Diabetes in Control articles.
How to Prevent a Diabetic Stroke
Preventing a diabetic stroke requires a multi-pronged approach that includes medical, lifestyle, and dietary interventions. Fortunately, many of the steps that reduce stroke risk also help manage diabetes more effectively.
1. Monitor and Control Blood Sugar:
Keeping your A1C under 7% (or a target set by your doctor) reduces vessel damage. Use CGM devices, maintain medication schedules, and avoid prolonged hyperglycemia.
2. Manage Blood Pressure:
Aim for readings below 130/80 mmHg. Many diabetics need antihypertensives like lisinopril or losartan alongside lifestyle changes.
3. Lower LDL Cholesterol:
Statins like atorvastatin and rosuvastatin are often prescribed to keep LDL below 100 mg/dL—or even lower in high-risk patients.
4. Avoid Smoking and Excess Alcohol:
Both habits significantly increase stroke risk. If quitting feels overwhelming, seek support through Healthcare.pro to find nearby cessation programs or therapists.
5. Exercise Regularly:
Moderate physical activity, such as brisk walking for 30 minutes a day, five days a week, supports both blood sugar and cardiovascular health.
6. Healthy Diet Choices:
Focus on anti-inflammatory foods like leafy greens, omega-3-rich fish, nuts, and whole grains. Limit sodium, trans fats, and refined sugars.
7. Weight Management and Insulin Sensitivity:
Losing just 5–10% of your body weight can have a profound impact. Medications like Mounjaro or Ozempic may aid both weight loss and blood sugar control.
Above all, make sure to schedule regular checkups with your endocrinologist or primary care provider. Regular lab work, eye exams, and cardiovascular screenings can catch risk factors before they escalate.
Conclusion
A diabetic stroke is not a random occurrence—it’s the result of multiple risk factors converging over time. Fortunately, the same strategies that control blood sugar can also protect your brain. By understanding the warning signs, managing your ABCs, and staying committed to lifestyle changes, you can significantly lower your stroke risk.
Don’t wait for symptoms to appear before taking action. Prevention starts today—and it could save your life.
FAQs
What is the difference between a diabetic stroke and a regular stroke?
A diabetic stroke is essentially a stroke that occurs in someone with diabetes, but it’s more likely due to vascular complications caused by chronic high blood sugar.
Can high blood sugar alone cause a stroke?
High blood sugar contributes to vessel damage and clot formation, which can increase stroke risk, but it usually acts in combination with other factors like hypertension or cholesterol.
Are stroke symptoms different in people with diabetes?
They can be. Neuropathy may mask numbness, and hypoglycemia may cause confusion or vision problems similar to stroke symptoms. Always err on the side of caution and seek help.
What medications help reduce stroke risk in diabetics?
Statins, antihypertensives, and certain glucose-lowering drugs like Ozempic or Jardiance have shown cardiovascular benefits. Your doctor will help choose the best fit.
How often should I get screened for stroke risk?
At least annually—more frequently if you have multiple risk factors or a history of cardiovascular events. Talk to your doctor or visit Healthcare.pro for local specialists.
Disclaimer:
“This content is not medical advice. For any health issues, always consult a healthcare professional. In an emergency, call 911 or your local emergency services.”