Introduction
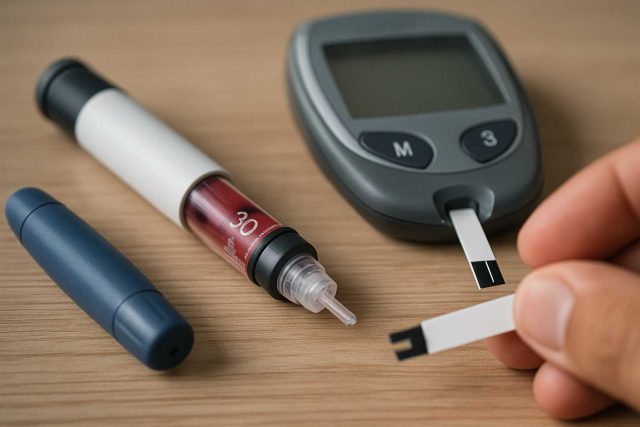
How far have we come in managing Type 1 Diabetes, and where are we headed next? In 2025, advancements in medical technology, digital health platforms, and pharmacologic innovations are reshaping the landscape of Type 1 Diabetes Management. From automated insulin delivery systems to adjunctive therapies like SGLT2 inhibitors, clinicians are now equipped with tools that not only improve glycemic control but also enhance patient quality of life. For healthcare professionals managing this chronic condition, staying ahead of these developments is not optional—it’s essential.
Table of Contents
- Advances in Insulin Therapy
- Artificial Pancreas and CGM Integration
- Adjunctive Medications and Innovations
- Behavioral and Digital Health Tools
- Conclusion
- FAQs
Advances in Insulin Therapy
The foundation of Type 1 Diabetes Management still rests on insulin therapy. However, today’s insulin options are far more refined than those of the past. Ultra-rapid-acting insulin analogs like Fiasp (faster-acting insulin aspart) have significantly reduced the postprandial glucose spike. Meanwhile, newer long-acting insulins, such as insulin degludec (Tresiba), offer flexible dosing schedules and a lower risk of nocturnal hypoglycemia.
Combination basal-bolus regimens are evolving as well. Personalized insulin-to-carb ratios and correction factors supported by AI algorithms are making insulin dosing more precise than ever. Transitioning patients to these regimens requires provider education and close monitoring, but the clinical payoff is often substantial.
Artificial Pancreas and CGM Integration
One of the most promising developments is the rise of hybrid closed-loop systems, commonly referred to as artificial pancreas technology. Devices like the Medtronic MiniMed 780G and Tandem t:slim X2 with Control-IQ combine continuous glucose monitoring (CGM) with automated insulin delivery.
These systems reduce the burden of daily management while improving Time in Range (TIR) metrics. According to a 2024 study published in The Lancet Diabetes & Endocrinology, patients using closed-loop systems had a 20% improvement in TIR compared to those on traditional pump therapy.
Moreover, sensor accuracy continues to improve. The latest generation of CGMs like Dexcom G7 and FreeStyle Libre 3 offer shorter warm-up times, better accuracy, and direct smartphone integration—further empowering patients to engage with their data in real-time.
Adjunctive Medications and Innovations
While insulin remains essential, several adjunctive treatments are being explored to improve metabolic outcomes. SGLT2 inhibitors like dapagliflozin and empagliflozin, though primarily approved for Type 2 Diabetes, are being studied for their benefits in Type 1 Diabetes.
These agents have shown promise in reducing glycemic variability, body weight, and even cardiovascular risk. However, the risk of diabetic ketoacidosis (DKA) necessitates careful patient selection and education. Ongoing trials are refining these protocols.
Additionally, immunotherapy aimed at preserving beta-cell function is under investigation. Drugs like teplizumab are paving the way for early intervention, potentially altering the disease’s progression when administered during the honeymoon phase.
Behavioral and Digital Health Tools
While clinical advancements are critical, so is patient behavior. Mobile applications, such as mySugr and Glooko, are supporting both patient education and clinician workflow integration. These platforms allow real-time data sharing, which can be especially valuable in remote care settings.
Mental health tools tailored to people with diabetes, such as digital CBT programs and peer support networks, are gaining traction. They address diabetes distress and promote adherence—key components of successful Type 1 Diabetes Management.
Telemedicine, initially a stopgap during the pandemic, has now become a staple. Many endocrinology practices are leveraging platforms like Doximity Dialer and Amwell to follow up with patients, review glucose trends, and adjust medications—all without in-person visits.
Conclusion
The face of Type 1 Diabetes Management is transforming, thanks to technological, pharmacological, and behavioral innovations. Clinicians who stay updated on these advancements are better positioned to offer comprehensive, individualized care. Although challenges remain, the toolkit for managing Type 1 Diabetes in 2025 is more robust than ever, promising brighter outcomes for patients navigating this lifelong condition.
For more updates on diabetes management, visit Diabetes in Control and HealingWell’s Diabetes Forum.
Frequently Asked Questions
What is the latest insulin option available for Type 1 Diabetes?
Ultra-rapid insulins like Fiasp and long-acting options like Tresiba are among the latest innovations, offering improved flexibility and control.
Are SGLT2 inhibitors approved for use in Type 1 Diabetes?
While not FDA-approved specifically for Type 1, some clinicians are using them off-label with caution due to potential DKA risk.
What is a hybrid closed-loop system?
It’s an automated insulin delivery system that adjusts basal insulin based on CGM data, often referred to as an “artificial pancreas.”
How do digital apps help with diabetes management?
Apps support real-time monitoring, medication tracking, carbohydrate counting, and data sharing between patients and providers.
Is telemedicine effective for Type 1 Diabetes care?
Yes, it allows for timely follow-ups, glucose trend analysis, and medication adjustments with convenience and efficiency.
Disclaimer
“This content is not medical advice. For any health issues, always consult a healthcare professional. In an emergency, call 911 or your local emergency services.”