Imagine being at a fork in the road—one path leads to type 2 diabetes, the other to a healthier future. That’s the crossroads of prediabetes. Although it may not come with obvious symptoms, it’s a crucial warning sign. Prediabetes management is where prevention begins, and the sooner it’s addressed, the more effective the results.
More than 96 million American adults are estimated to have prediabetes, but most don’t know it. Left unaddressed, prediabetes often progresses to full-blown diabetes. However, with the right interventions, it doesn’t have to. Doctors know what works, and in this article, we’ll reveal the practical, science-backed secrets that healthcare providers want every patient to know.
Table of Contents
- Why Early Prediabetes Management Is Critical
- Key Lifestyle Interventions That Work
- Medications and Monitoring: What to Consider
- The Role of Mental Health and Support Systems
- Conclusion and FAQs
Why Early Prediabetes Management Is Critical
When patients hear the term “prediabetes,” they often assume it’s a mild concern. But doctors view it differently. It’s not just a gray area—it’s a flashing yellow light.
Prediabetes means your blood sugar levels are higher than normal but not yet in the diabetic range. Specifically, a fasting blood glucose between 100–125 mg/dL or an A1C of 5.7%–6.4% indicates risk. However, it also means there’s a significant opportunity to intervene.
The reason early action matters is that insulin resistance—one of the key drivers of prediabetes—can be slowed or reversed. With targeted lifestyle changes, patients can reduce their risk of developing type 2 diabetes by over 50%, according to the CDC’s Diabetes Prevention Program.
Doctors emphasize that waiting until you feel symptoms is a mistake. Most people don’t feel any different during the early stages. That’s why annual screenings are vital, especially for those with family history, obesity, or sedentary lifestyles.
To stay informed on emerging research and tips, visit Diabetes in Control’s article archive.
Key Lifestyle Interventions That Work
Lifestyle changes are the cornerstone of effective prediabetes management. While that might sound like standard advice, it’s rooted in solid science and clinical experience.
1. Nutrition Overhaul
Doctors don’t usually recommend extreme diets. Instead, they advise gradual, sustainable changes. Reducing added sugars and refined carbs while increasing fiber-rich foods can help regulate blood sugar levels. Many providers now recommend the Mediterranean diet or a lower-carb approach to balance glucose and insulin response.
2. Weight Loss—Even Small Amounts Matter
Losing just 5–7% of your body weight can significantly reduce insulin resistance. For someone weighing 200 pounds, that’s only 10–14 pounds. Small progress makes a big difference.
3. Exercise as Medicine
Regular physical activity improves insulin sensitivity. Doctors typically recommend 150 minutes per week of moderate aerobic activity, such as brisk walking. Resistance training twice a week also helps regulate glucose levels by building muscle, which absorbs more sugar.
4. Sleep and Stress Management
Chronic stress and poor sleep disrupt hormones and raise blood sugar. Mindfulness, breathing exercises, and consistent sleep routines are now standard parts of treatment plans.
It’s no longer just about avoiding sugar—it’s about optimizing your body’s ability to use insulin effectively.
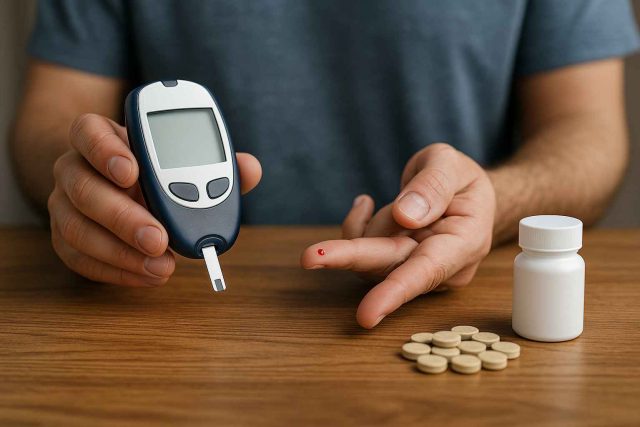
Medications and Monitoring: What to Consider
While lifestyle remains the primary tool for reversing prediabetes, doctors are increasingly turning to medications in high-risk cases. These aren’t shortcuts—they’re supplements to behavior change.
1. Metformin
Metformin is often prescribed off-label for prediabetes, especially for patients who are overweight or have other risk factors. It improves insulin sensitivity and has a long track record of safety. Studies show it can reduce progression to diabetes by 31%, with even better results when combined with lifestyle changes.
2. GLP-1 Receptor Agonists
Medications like Ozempic (semaglutide) and Mounjaro (tirzepatide), while primarily indicated for type 2 diabetes, are being explored for prediabetes due to their benefits in weight loss and blood sugar control. Clinical trials continue to show promise for using these therapies earlier in the disease trajectory.
3. Continuous Glucose Monitoring (CGM)
Though traditionally reserved for diagnosed diabetics, CGMs like Dexcom G7 or Freestyle Libre are being used in prediabetic patients to promote real-time awareness and behavior modification. Doctors find that when patients can see how specific meals or stressors affect their glucose, they make better choices.
It’s important to consult a qualified provider before starting any new medication. For help finding a specialist near you, visit Healthcare.pro.
The Role of Mental Health and Support Systems
One of the most overlooked components of prediabetes management is mental health. Behavior change is hard—and it’s even harder without the right mindset and support.
Depression, anxiety, and emotional eating often interfere with long-term success. Doctors increasingly refer patients to behavioral counselors, diabetes educators, and support groups to address the psychological side of lifestyle change.
Group-based diabetes prevention programs—offered in-person or virtually—are particularly effective. Participants learn strategies, set goals, and hold each other accountable. Studies show they are nearly twice as likely to reduce their diabetes risk compared to those managing it alone.
Additionally, digital tools now make it easier to stay on track. Mobile apps that track food, exercise, sleep, and stress can sync with wearable devices and alert healthcare teams when patterns change. Many doctors are now incorporating these platforms into personalized care plans.
Ultimately, sustainable prediabetes management requires more than willpower—it requires community, feedback, and a plan that adjusts as life changes.
Conclusion and FAQs
Prediabetes isn’t the end of the road—it’s a chance to take back control. With early action, smart lifestyle changes, and when needed, medical support, patients can dramatically reduce their risk of progressing to type 2 diabetes.
Doctors want patients to understand that small, consistent choices create long-term protection. The key is not waiting until it’s too late.
FAQs
Can prediabetes be reversed permanently?
Yes, with sustained lifestyle changes, many people return to normal blood sugar levels. However, ongoing monitoring is important to prevent relapse.
Is medication necessary for managing prediabetes?
Not always. Lifestyle changes are often enough. However, medications like metformin or GLP-1 agonists may be used in high-risk individuals.
How often should I check my blood sugar with prediabetes?
Doctors may recommend periodic A1C testing and self-monitoring, especially if you’re trying a new diet or medication. CGMs offer real-time insights for some patients.
What are the biggest lifestyle factors for reversing prediabetes?
Diet, weight loss, regular exercise, quality sleep, and stress reduction are the most influential factors for reversing insulin resistance.
Should I see a specialist for prediabetes?
A primary care provider can often manage prediabetes, but an endocrinologist or diabetes educator may be helpful for customized care.
Disclaimer
This content is not medical advice. For any health issues, always consult a healthcare professional. In an emergency, call 911 or your local emergency services.