Introduction
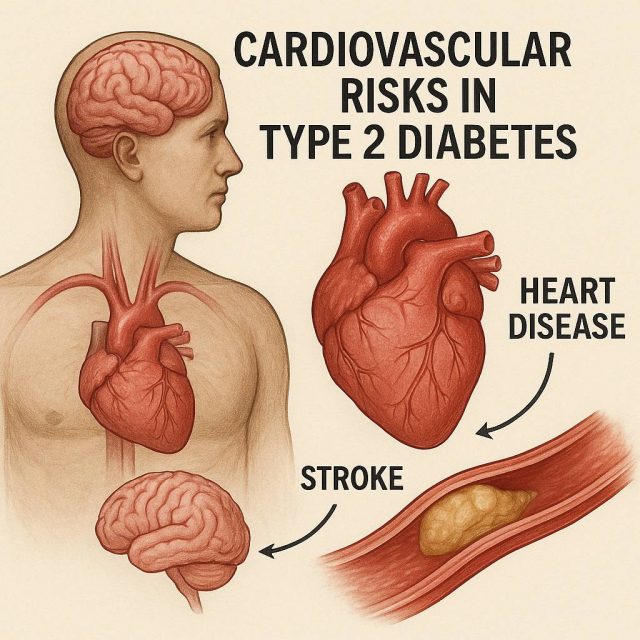
When we think about Type 2 diabetes, blood sugar control usually takes center stage. Yet, beneath the surface lies a more pressing danger—cardiovascular risks in Type 2 diabetes that silently drive heart disease, stroke, and early mortality. What if the real threat to patients was not their glucose readings, but the hidden vascular damage accumulating over years?
Providers navigating modern diabetes care must look beyond HbA1c. Cardiovascular complications remain the leading cause of death in this population, and emerging evidence shows the need for earlier, proactive intervention. In this article, we will explore the overlooked risks, the role of modern therapies like GLP-1 receptor agonists and SGLT2 inhibitors, and the practical steps every provider should prioritize.
Table of Contents
- Understanding the Overlap of Diabetes and Heart Disease
- Why Cardiovascular Risks in Type 2 Diabetes Remain Underestimated
- Modern Therapeutics and Their Impact on Cardiovascular Health
- Practical Steps Providers Can Take Today
- Conclusion and FAQs
Understanding the Overlap of Diabetes and Heart Disease
The relationship between Type 2 diabetes and cardiovascular disease is not coincidental. Insulin resistance, chronic inflammation, and endothelial dysfunction all converge to increase a patient’s vulnerability to heart failure, atherosclerosis, and myocardial infarction. Research consistently shows that adults with Type 2 diabetes are two to four times more likely to develop cardiovascular disease compared to those without diabetes (American Heart Association).
Despite this known association, providers often focus primarily on glycemic management. While lowering HbA1c is vital, it does not fully address the mechanisms driving cardiovascular harm. Elevated triglycerides, low HDL cholesterol, and hypertension remain silent contributors to risk. Moreover, lifestyle factors such as sedentary behavior and dietary imbalances compound the challenge.
Understanding this overlap is critical because it reframes the treatment approach. Instead of viewing cardiovascular events as downstream complications, they should be seen as parallel targets for prevention from the moment of diagnosis.
Why Cardiovascular Risks in Type 2 Diabetes Remain Underestimated
Why are cardiovascular risks in Type 2 diabetes often underestimated? Part of the issue lies in the subtle progression of vascular disease. Patients can feel fine even while plaque builds in their arteries. By the time symptoms appear, damage is often irreversible.
Another factor is fragmented care. Endocrinologists, cardiologists, and primary care providers may not always align on prevention strategies. Without coordinated screening and intervention, gaps emerge. This lack of integration means many patients miss early opportunities for cardiovascular protection.
Additionally, traditional metrics have created blind spots. Providers may celebrate reduced HbA1c levels without noticing ongoing hypertension or dyslipidemia. The focus on glucose alone has historically overshadowed broader cardiovascular management.
Recent studies highlight this gap. For example, trials such as EMPA-REG and LEADER demonstrated that SGLT2 inhibitors like Jardiance (empagliflozin) and GLP-1 receptor agonists like Victoza (liraglutide) significantly reduce cardiovascular events independent of blood sugar control. This underscores the need for providers to expand their focus beyond glucose numbers.
Modern Therapeutics and Their Impact on Cardiovascular Health
The therapeutic landscape for Type 2 diabetes has shifted dramatically in the past decade. No longer are treatments judged solely on their ability to lower glucose. Now, providers must weigh cardiovascular outcomes just as heavily.
SGLT2 inhibitors such as Jardiance, Farxiga (dapagliflozin), and Invokana (canagliflozin) have reshaped the treatment paradigm. These agents not only lower blood sugar but also reduce hospitalizations for heart failure and slow the progression of chronic kidney disease. Their role in reducing cardiovascular mortality has been a game-changer in diabetes care.
GLP-1 receptor agonists like Ozempic (semaglutide), Trulicity (dulaglutide), and Victoza offer similar benefits, particularly in reducing the risk of major adverse cardiovascular events. These medications are increasingly recommended as first-line therapy for patients with established cardiovascular disease or high risk.
However, these advances require proactive adoption. Providers must feel comfortable initiating these therapies and counseling patients about their long-term benefits. This represents a shift from reactive treatment to anticipatory care, prioritizing cardiovascular health as much as glycemic control.
For clinicians seeking deeper insight into how these therapies shape patient outcomes, resources such as Diabetes in Control articles provide valuable updates on evolving treatment strategies.
Practical Steps Providers Can Take Today
What does this mean for everyday practice? Providers need actionable strategies that address both metabolic and cardiovascular health simultaneously.
First, risk assessment should become routine at diagnosis. Checking lipid profiles, blood pressure, and family history of cardiovascular disease can guide early intervention. Second, encourage patients to adopt lifestyle modifications with proven benefits, including the DASH diet, increased physical activity, and smoking cessation. While these steps may sound basic, they significantly lower cardiovascular event rates.
Third, medication choices matter. Incorporating SGLT2 inhibitors and GLP-1 receptor agonists earlier in the treatment algorithm can save lives. Instead of reserving these drugs for advanced cases, providers should consider them earlier for patients with multiple risk factors.
Fourth, education and shared decision-making remain central. Patients are more likely to adhere to therapy when they understand not just its impact on blood sugar, but also its ability to prevent heart attacks and strokes. Directing patients to reliable resources like Healthcare.pro can reinforce these messages and provide support outside of clinic visits.
Finally, collaboration across specialties is essential. Providers who engage cardiologists and nephrologists in a coordinated care plan will achieve better outcomes than those working in silos. Interdisciplinary care not only closes gaps but also ensures patients benefit from the full range of available interventions.
Conclusion
Cardiovascular risks in Type 2 diabetes are not secondary complications but central threats that demand provider attention from day one. By broadening the focus beyond glucose control, embracing modern therapeutics, and prioritizing collaboration, clinicians can significantly reduce mortality and improve patient quality of life. The silent progression of vascular damage requires vigilance, but with proactive strategies, providers can shift the trajectory of care for millions living with diabetes.
FAQs
Why are patients with Type 2 diabetes at higher risk for heart disease?
Diabetes accelerates vascular damage through inflammation, insulin resistance, and lipid abnormalities, all of which increase the likelihood of cardiovascular events.
Which medications reduce cardiovascular risks in Type 2 diabetes?
SGLT2 inhibitors like Jardiance and GLP-1 receptor agonists like Ozempic have been shown to significantly reduce cardiovascular events beyond glucose lowering.
Should cardiovascular risk assessment start at diagnosis?
Yes. Providers should evaluate blood pressure, lipid levels, and other risk factors at the time of diagnosis to guide early preventive strategies.
How can providers encourage patient adherence to cardiovascular-focused therapies?
By explaining the dual benefits of these medications—blood sugar control and cardiovascular protection—patients are more likely to stay engaged with treatment.
Are lifestyle changes still effective in reducing cardiovascular risks?
Absolutely. Diet, exercise, and smoking cessation remain cornerstones of prevention, even when advanced therapies are used.
Disclaimer:
This content is not medical advice. For any health issues, always consult a healthcare professional. In an emergency, call 911 or your local emergency services.