HIV remains a critical public health challenge around the globe. However, HIV prevention has become more effective and accessible than ever before. With a variety of tools and strategies available, patients can take proactive steps to protect themselves. But how do we distinguish fact from fiction in a sea of information?
Table of Contents
- What is HIV and How is it Transmitted?
- Proven HIV Prevention Methods
- Medical Interventions: PrEP and PEP
- Behavioral and Community-Based Approaches
- Conclusion
- FAQs
What is HIV and How is it Transmitted?
Human Immunodeficiency Virus (HIV) is a virus that weakens the immune system, making individuals more susceptible to infections and certain cancers. Left untreated, HIV can progress to Acquired Immunodeficiency Syndrome (AIDS), a condition characterized by a severely compromised immune response.
HIV is primarily transmitted through specific bodily fluids such as blood, semen, vaginal fluids, rectal fluids, and breast milk. Most transmissions occur through unprotected sex, sharing of needles, or from mother to child during childbirth or breastfeeding. Casual contact like hugging or sharing utensils does not spread the virus.
Understanding how HIV is transmitted is the first step in implementing effective HIV prevention strategies. By reducing exposure to the virus, individuals can significantly lower their risk.
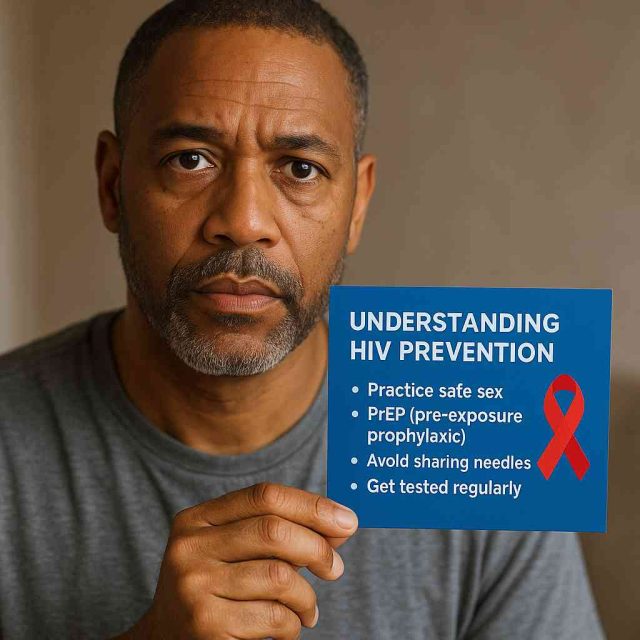
Proven HIV Prevention Methods
Successful HIV prevention involves a combination of practices that address various risk factors. Consistent and correct use of condoms is among the most effective ways to prevent transmission during sex. Latex condoms offer a physical barrier that blocks the virus, reducing the chance of exposure.
Routine HIV testing is another cornerstone of prevention. Early detection not only improves outcomes for those who are positive but also prevents transmission to others. Individuals who know their status can make informed choices and access treatment if needed.
Needle exchange programs also play a vital role, particularly for individuals who inject drugs. By providing clean syringes, these programs reduce the risk of HIV transmission from contaminated needles. Education about safe injection practices further supports harm reduction.
Moreover, community education programs are essential. These initiatives raise awareness, reduce stigma, and empower individuals with accurate information. Read more about community-based strategies at AIDS.org Blog.
Medical Interventions: PrEP and PEP
In recent years, antiretroviral medications have become an integral part of HIV prevention. Pre-exposure prophylaxis (PrEP) is a daily pill for people at high risk of HIV. When taken consistently, PrEP can reduce the risk of infection from sex by about 99% and from injection drug use by at least 74%.
Common PrEP medications include brand names like Truvada and Descovy. These drugs work by preventing the virus from establishing a permanent infection if exposure occurs. However, PrEP is most effective when combined with other prevention strategies like condom use.
Post-exposure prophylaxis (PEP) is another tool. It involves taking antiretroviral medicines after a potential HIV exposure. PEP must be started within 72 hours and continued for 28 days. It’s typically used in emergency situations, such as after unprotected sex or needle-sharing incidents.
These interventions require a prescription and medical supervision. Patients interested in PrEP or PEP should consult a healthcare provider or visit Healthcare.pro for guidance.
Behavioral and Community-Based Approaches
Behavioral changes remain crucial in reducing HIV risk. Open communication with sexual partners about HIV status and prevention methods fosters safer interactions. Limiting the number of sexual partners and avoiding high-risk behaviors like sharing needles further decreases exposure.
Stigma around HIV can discourage individuals from seeking prevention tools. Community-based support groups, educational workshops, and online platforms help break down these barriers. Additionally, promoting inclusive sex education in schools can start important conversations early.
Faith-based and cultural organizations can also support HIV prevention through outreach, testing events, and awareness campaigns. These groups often have trusted relationships with their communities and can tailor messages to meet local needs.
For more information about our Mission visit AIDS.org FAQs. Staying informed and engaged is one of the most powerful forms of prevention.
Conclusion
HIV prevention has never been more effective or more critical. From medical treatments like PrEP and PEP to behavioral changes and community outreach, there are numerous ways for patients to protect themselves. Understanding HIV transmission, practicing safe behaviors, and accessing healthcare resources empower individuals to stay ahead of the virus.
FAQs
What is the most effective HIV prevention method?
While no method is 100% foolproof, using condoms and taking PrEP consistently offers the highest level of protection.
Can you take PrEP if you don’t have HIV?
Yes, PrEP is specifically for HIV-negative individuals who are at higher risk of exposure.
How soon after exposure should you take PEP?
PEP should be started within 72 hours of potential exposure. The sooner, the better.
Do HIV prevention methods have side effects?
Some individuals experience mild side effects like nausea with PrEP or PEP, but these usually subside.
Where can I get tested or learn more?
Visit local health clinics or access information at Healthcare.pro or AIDS.org Blog.
“This content is not medical advice. For any health issues, always consult a healthcare professional. In an emergency, call 911 or your local emergency services.”