Sugar molecules are often seen as the body’s simplest energy source, yet their relationship with type 1 diabetes is far more complex. When functioning normally, sugar molecules provide glucose, the primary fuel for the brain, muscles, and organs. In type 1 diabetes, however, the way the body processes and regulates sugar molecules changes dramatically. Without insulin, the hormone needed to move glucose into cells, sugar molecules build up in the bloodstream instead of being used for energy. But what role do these molecules play in triggering type 1 diabetes, and how might understanding them reshape treatment strategies?
Table of Contents
- How Sugar Molecules Work in the Body
- The Link Between Sugar Molecules and Type 1 Diabetes
- Advances in Research on Sugar Metabolism and Autoimmunity
- Implications for Treatment and Future Directions
- Conclusion
- FAQs
How Sugar Molecules Work in the Body
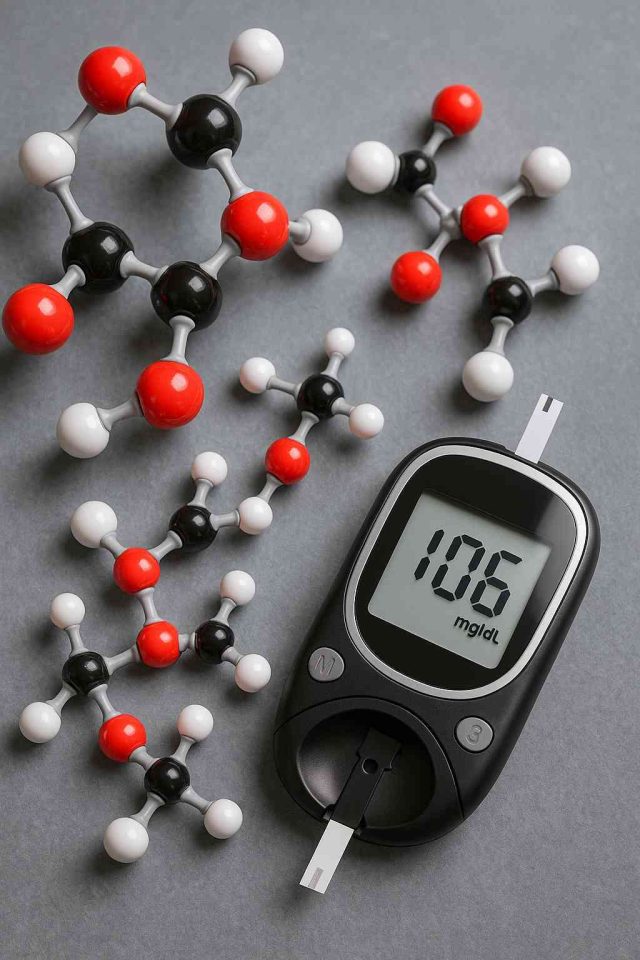
Sugar molecules, also known as saccharides, come in different forms—glucose, fructose, lactose, and sucrose. Glucose is the most significant for human health, since it is the body’s primary energy source. After meals, carbohydrates are broken down into sugar molecules, which enter the bloodstream and supply fuel to cells.
Normally, the pancreas releases insulin to help transport glucose into tissues where it is stored or used. However, in type 1 diabetes, the immune system attacks the beta cells in the pancreas that produce insulin. Without insulin, sugar molecules accumulate in the blood, causing hyperglycemia. This buildup can lead to dangerous complications like diabetic ketoacidosis (DKA), nerve damage, and vision loss if not managed.
It’s important to note that sugar molecules themselves are not the enemy. They are vital for survival. The problem arises when insulin is missing, making it impossible for the body to regulate glucose effectively. Understanding how sugar molecules behave under these conditions is crucial for clinicians who want to improve diabetes management strategies.
The Link Between Sugar Molecules and Type 1 Diabetes
The connection between sugar molecules and type 1 diabetes goes beyond high blood glucose. Researchers have discovered that sugar molecules also play a role in immune regulation. Specific glycans, which are complex sugar structures on proteins and cell surfaces, appear to influence how the immune system recognizes and responds to the body’s tissues.
For example, autoantibodies often target proteins that are coated with sugar molecules. These interactions may help explain why the immune system mistakenly attacks pancreatic beta cells. In fact, studies suggest that abnormal glycosylation patterns—a process where sugar molecules attach incorrectly to proteins—might contribute to the onset of type 1 diabetes.
Another important link lies in metabolism. When glucose cannot enter cells, the body breaks down fat for fuel, leading to the production of ketones. While ketones provide energy, excess production results in ketoacidosis, a life-threatening complication. Thus, the way sugar molecules interact with insulin—or fail to—determines whether patients remain stable or enter crisis.
The clinical takeaway is that sugar molecules influence both the metabolic and immune aspects of type 1 diabetes. This dual role makes them central to understanding why the disease develops and how it can be controlled. For more clinical discussions, Diabetes in Control articles provide updated perspectives on these mechanisms.
Advances in Research on Sugar Metabolism and Autoimmunity
In recent years, research has focused on how sugar molecules might unlock new treatments for type 1 diabetes. Scientists are exploring the concept of glycoimmunology, which studies how glycans influence immune responses. By altering sugar molecule patterns on immune cells, it may be possible to reduce autoimmune attacks against the pancreas.
Furthermore, advancements in continuous glucose monitoring (CGM) have provided detailed insights into how sugar molecules fluctuate daily. Devices like Dexcom G7 and Abbott’s FreeStyle Libre 3 allow real-time tracking of glucose, helping patients and providers detect patterns that traditional A1C tests might miss. These innovations have reshaped diabetes care by making it easier to match insulin therapy to glucose trends.
Experimental therapies are also emerging. Some studies are testing engineered proteins that mimic natural sugar molecule patterns, with the goal of retraining the immune system to tolerate pancreatic beta cells. Others are examining how dietary interventions might alter gut microbiota and their relationship to glucose metabolism.
The combination of biology and technology creates new opportunities. If researchers can fully understand how sugar molecules interact with the immune system, they may uncover pathways to delay or prevent type 1 diabetes altogether.
Implications for Treatment and Future Directions
For patients and providers, understanding sugar molecules has practical implications. Improved knowledge of how sugar molecules influence both metabolism and immunity could lead to more personalized treatment strategies. Instead of a one-size-fits-all approach, clinicians may soon tailor insulin regimens, diets, and adjunct therapies based on a patient’s individual glycan patterns and glucose fluctuations.
Digital health is already enhancing this personalization. Smartphone apps integrated with CGMs provide alerts for high or low glucose, helping patients respond quickly. Data-sharing platforms enable providers to track trends and adjust treatment remotely. This level of integration gives patients a clearer view of how sugar molecules behave in their own bodies on a daily basis.
Pharmacological advances also hold promise. Branded drugs like insulin analogs (Humalog, Novolog) and adjuncts like pramlintide work more effectively when paired with continuous monitoring. As new drugs enter the pipeline, the role of sugar molecules in both absorption and action will likely remain a key focus.
Looking ahead, the ultimate goal is to prevent type 1 diabetes altogether. Vaccines, immune therapies, and precision medicine approaches are all under investigation. While a cure remains elusive, the growing understanding of sugar molecules offers hope for interventions that could preserve beta cell function or delay disease progression.
For patients seeking to better manage diabetes today, practical education remains essential. Resources like Healthcare.pro can help patients learn how to interpret their glucose data, discuss it with providers, and make informed lifestyle changes.
Conclusion
Sugar molecules are more than simple energy units. They sit at the intersection of metabolism and immunity, shaping how type 1 diabetes develops and progresses. Advances in glycoimmunology, continuous glucose monitoring, and digital health tools are helping clinicians and patients see the full picture of how sugar molecules affect the body.
As research continues, the future holds exciting possibilities for targeted therapies and even preventive strategies. By better understanding sugar molecules, we move closer to a world where type 1 diabetes is not only manageable but potentially preventable.
FAQs
What role do sugar molecules play in type 1 diabetes?
They provide energy but, without insulin, accumulate in the bloodstream, causing high blood glucose and complications.
Are sugar molecules responsible for triggering autoimmunity?
Research suggests abnormal sugar molecule patterns on proteins may contribute to immune system attacks on the pancreas.
How do continuous glucose monitors help track sugar molecules?
They provide real-time data on glucose levels, helping patients and providers manage fluctuations more effectively.
Can sugar molecules be targeted for new treatments?
Yes. Experimental therapies aim to modify glycan patterns to retrain the immune system and protect beta cells.
Will better understanding of sugar molecules lead to a cure for type 1 diabetes?
Not yet, but it could lead to therapies that delay onset, preserve beta cells, or personalize treatment strategies.
“This content is not medical advice. For any health issues, always consult a healthcare professional. In an emergency, call 911 or your local emergency services.”