Is your A1C at 7 percent? If you’re living with Type 2 diabetes, this number isn’t just a lab result—it’s a critical snapshot of how well your blood sugar has been controlled over time. Think of A1C like a “grade” on your diabetes report card. But what exactly does it mean, and is 7% considered good or bad?
Let’s break down this essential diabetes marker, explore what drives it, and uncover how it can inform better diabetes management strategies—especially for patients, caregivers, and clinicians navigating Type 2 diabetes.
Table of Contents
- What Is A1C and Why It Matters
- Is an A1C of 7 Percent Good or Bad?
- Managing A1C: Lifestyle, Medication & Monitoring
- When A1C Isn’t the Whole Story
What Is A1C and Why It Matters
The A1C test, also called the hemoglobin A1C or HbA1c test, measures the average blood glucose (blood sugar) level over the past two to three months. It works by identifying the percentage of glycated hemoglobin—hemoglobin that has sugar attached to it.
Why does this matter? Because the more glucose in your bloodstream, the higher your A1C will be. This test offers a long-term view of glycemic control, unlike a daily glucose check, which is only a snapshot.
For people with Type 2 diabetes, the A1C test is a cornerstone for diagnosis and monitoring. According to the American Diabetes Association (ADA), an A1C of 6.5% or higher typically signals diabetes, while levels between 5.7% and 6.4% indicate prediabetes.
Is an A1C of 7 Percent Good or Bad?
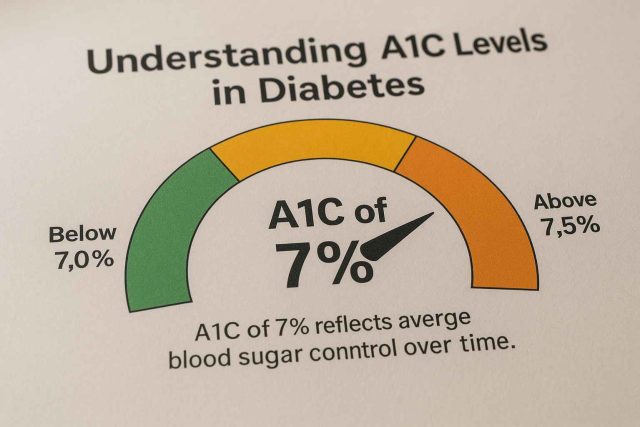
An A1C of 7 percent is often seen as a “golden target” for many adults with diabetes. But context matters. The ADA recommends a general A1C goal of less than 7% to reduce the risk of diabetes-related complications such as neuropathy, nephropathy, and retinopathy.
Still, the target A1C isn’t one-size-fits-all. Here’s how it breaks down:
- Good Control: An A1C of 7% typically equates to an estimated average glucose (eAG) of 154 mg/dL. This suggests relatively stable glucose management.
- Moderate Risk: Levels above 7.5% indicate rising blood sugar and an increased risk of complications.
- Tight Control: Some younger or newly diagnosed individuals may aim for 6.5% or even lower—if they can do so safely without hypoglycemia.
However, older adults or those with multiple comorbidities may benefit from a slightly higher target (e.g., 7.5–8.0%) to avoid the risks of low blood sugar.
It’s important to personalize the target A1C in consultation with a healthcare provider. You can explore more detailed discussions on patient-centered goals at Healthcare.pro.
Managing A1C: Lifestyle, Medication & Monitoring
Getting to a 7% A1C—and staying there—requires consistent effort. A multi-pronged approach usually works best.
1. Diet and Nutrition
Balanced nutrition is a game-changer. For instance, the Mediterranean diet and low-carb meal plans can significantly improve blood sugar. Incorporating more non-starchy vegetables, lean proteins, and whole grains helps stabilize post-meal spikes.
2. Physical Activity
Exercise helps lower A1C by improving insulin sensitivity. Aiming for 150 minutes of moderate aerobic activity weekly is a strong starting point. This could include brisk walking, swimming, or cycling.
3. Glucose Monitoring
Whether through finger-stick meters or continuous glucose monitors (CGMs), regular tracking provides actionable insights. CGMs in particular offer real-time data to adjust insulin or carb intake effectively.
4. Medication
For many, lifestyle changes aren’t enough. A range of medications can assist in lowering A1C:
- Metformin: Often the first-line oral drug.
- GLP-1 receptor agonists: Such as semaglutide (Ozempic, Wegovy) help both blood sugar and weight loss.
- SGLT2 inhibitors: Like empagliflozin (Jardiance) and canagliflozin (Invokana), support glucose control and heart health.
- Insulin therapy: Still essential for some, especially if A1C is well above target.
Individualized treatment plans ensure that interventions align with the patient’s health status and goals.
Want to dive deeper into medication strategies? Visit Diabetes in Control’s medication insights for updates and clinical perspectives.
When A1C Isn’t the Whole Story
Although A1C is a helpful metric, it’s not infallible. It reflects average glucose levels but doesn’t show glucose variability—how often and how severely your blood sugar swings.
In addition, A1C results can be skewed by:
- Anemia or other blood disorders
- Chronic kidney disease
- Certain ethnic or genetic factors affecting hemoglobin
Moreover, relying solely on A1C can mask episodes of hypoglycemia. For this reason, many endocrinologists recommend pairing A1C with Time in Range (TIR) metrics from CGMs, offering a more comprehensive picture of control.
Patients should also consider psychosocial aspects. Diabetes burnout, food insecurity, or access to care can all influence A1C outcomes.
If you’re unsure whether your A1C goal is right for you, a detailed conversation with your provider or a diabetes care team can offer clarity and direction.
Conclusion
An A1C of 7 percent is a meaningful benchmark in Type 2 diabetes care—representing well-managed blood sugar for many. But numbers never tell the whole story. Individual goals, lifestyle, and medical needs all influence what “success” looks like. By staying informed and proactive, patients can use A1C as a guide rather than a verdict.
FAQs
What does an A1C of 7 mean in terms of daily blood sugar?
It corresponds to an estimated average glucose of about 154 mg/dL over the past 2–3 months.
Can I lower my A1C without medication?
Yes, many people reduce A1C through diet, exercise, and weight loss. However, medication may still be needed depending on individual risk factors.
How often should I get my A1C checked?
Typically, every 3 to 6 months. More frequent testing may be necessary if your treatment plan is changing or your numbers are off-target.
Is 7% too high for someone with Type 2 diabetes?
Not necessarily. For many adults, it’s a recommended target. But your ideal goal may be slightly higher or lower based on your overall health.
What’s more important: A1C or daily glucose readings?
Both matter. A1C gives a long-term picture, while daily readings help manage short-term spikes and trends.
Disclaimer
This content is not medical advice. For any health issues, always consult a healthcare professional. In an emergency, call 911 or your local emergency services.