Have you or someone you know developed unusual movements of the face, tongue, or limbs after taking medication for mental health? These symptoms might be a sign of tardive dyskinesia, a condition that often flies under the radar but affects thousands of people each year.
Tardive dyskinesia is a neurological movement disorder that usually results from long-term use of antipsychotic medications. It involves involuntary, repetitive movements that can affect the face, mouth, torso, and extremities. While it can be frustrating or even embarrassing, understanding the condition is the first step toward managing it effectively.
Table of Contents
- What Causes Tardive Dyskinesia?
- Recognizing the Symptoms
- Treatment and Medication Options
- Living with Tardive Dyskinesia
- Conclusion and FAQs
What Causes Tardive Dyskinesia?
Tardive dyskinesia is most commonly linked to the prolonged use of dopamine-blocking drugs, especially first-generation antipsychotics like haloperidol and chlorpromazine. However, newer second-generation antipsychotics, such as risperidone or olanzapine, may also pose some risk.
These medications are often prescribed to manage conditions like schizophrenia, bipolar disorder, and severe depression. Over time, they can cause changes in how dopamine functions in the brain, leading to involuntary movements.
Some non-psychiatric drugs used for nausea, like metoclopramide, have also been implicated. Although less common, these cases still highlight the importance of reviewing all long-term medications with a healthcare provider.
Risk factors for tardive dyskinesia include older age, female gender, and a history of diabetes or brain injury. Genetics may also play a role, but research is ongoing.
According to the National Institute of Neurological Disorders and Stroke (NINDS), early detection and proactive monitoring of symptoms are key to reducing long-term effects.
Recognizing the Symptoms
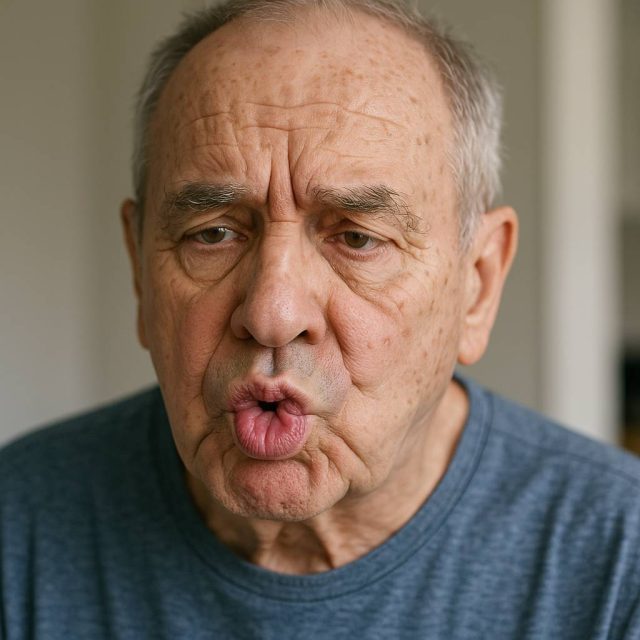
The signs of tardive dyskinesia can be subtle at first. Many patients report slight twitching or facial grimacing that gradually becomes more noticeable. These movements are involuntary, meaning the person cannot control or stop them.
Subheading: Common Symptoms of Tardive Dyskinesia
- Grimacing, lip smacking, or puckering
- Tongue protrusion or rapid tongue movements
- Blinking or eye movements
- Jerky arm, leg, or body movements
These symptoms can range from mild to severe and may worsen with stress or fatigue. In some cases, they interfere with speech, eating, or social interactions.
It’s important to distinguish tardive dyskinesia from other movement disorders like Parkinson’s disease or dystonia. A neurologist or psychiatrist will usually perform a physical exam and review medication history to make an accurate diagnosis.
Websites like Health.HealingWell.com can help patients connect with others and share symptom experiences.
Treatment and Medication Options
Once diagnosed, managing tardive dyskinesia often begins with reviewing the patient’s medication regimen. Adjusting or discontinuing the offending drug—under close medical supervision—can sometimes reduce symptoms.
Subheading: FDA-Approved Medications
Two medications approved specifically for tardive dyskinesia are Ingrezza (valbenazine) and Austedo (deutetrabenazine). These drugs work by regulating dopamine activity and have shown effectiveness in reducing involuntary movements.
Not everyone will respond the same way, so treatment plans must be individualized. In some cases, alternative psychiatric medications with a lower risk of movement disorders may be considered.
Physical therapy, stress management, and lifestyle modifications can complement drug therapy. A healthcare team might include a psychiatrist, neurologist, and primary care provider to ensure comprehensive care.
For those needing additional help locating specialists, Healthcare.pro offers access to licensed professionals with experience in managing complex movement disorders.
Living with Tardive Dyskinesia
Daily life with tardive dyskinesia presents unique challenges. The physical symptoms can lead to emotional stress, low self-esteem, or social withdrawal. However, many people find that a supportive environment and informed care plan make a huge difference.
Subheading: Emotional and Social Support
Talking openly with friends and family about tardive dyskinesia can reduce feelings of isolation. Joining a support group or online forum offers a place to share coping tips and hear from others facing similar experiences.
Workplace and educational accommodations may be necessary depending on the severity of symptoms. Advocacy groups often provide free resources, from legal guidance to educational brochures, to help people navigate these transitions.
Mindfulness practices, cognitive behavioral therapy (CBT), and relaxation techniques like yoga or deep breathing can improve quality of life. While these methods do not cure the condition, they help manage the psychological impact.
It’s also essential to maintain open communication with your healthcare team. Regular follow-ups can monitor for medication side effects, track progress, and make timely adjustments.
Conclusion
Tardive dyskinesia is a complex but manageable condition. By understanding the causes, recognizing early symptoms, and working with a knowledgeable healthcare team, patients can take proactive steps toward improved health and well-being.
Thanks to growing awareness and medical advancements, living a fulfilling life with tardive dyskinesia is not only possible—it’s increasingly common.
FAQs
What causes tardive dyskinesia?
It is usually caused by long-term use of dopamine-blocking medications, such as antipsychotics.
Is tardive dyskinesia permanent?
It can be long-lasting, but in some cases, symptoms may improve with treatment changes or medications like Ingrezza and Austedo.
Can younger people develop tardive dyskinesia?
Yes, although older adults are more at risk, young people taking certain medications can also be affected.
Are there natural remedies for tardive dyskinesia?
While no natural cure exists, relaxation techniques and supportive therapies may help with symptom management.
Where can I find a specialist?
You can search for licensed providers at Healthcare.pro or ask for referrals from your primary care physician.
This content is not medical advice. For any health issues, always consult a healthcare professional. In an emergency, call 911 or your local emergency services.