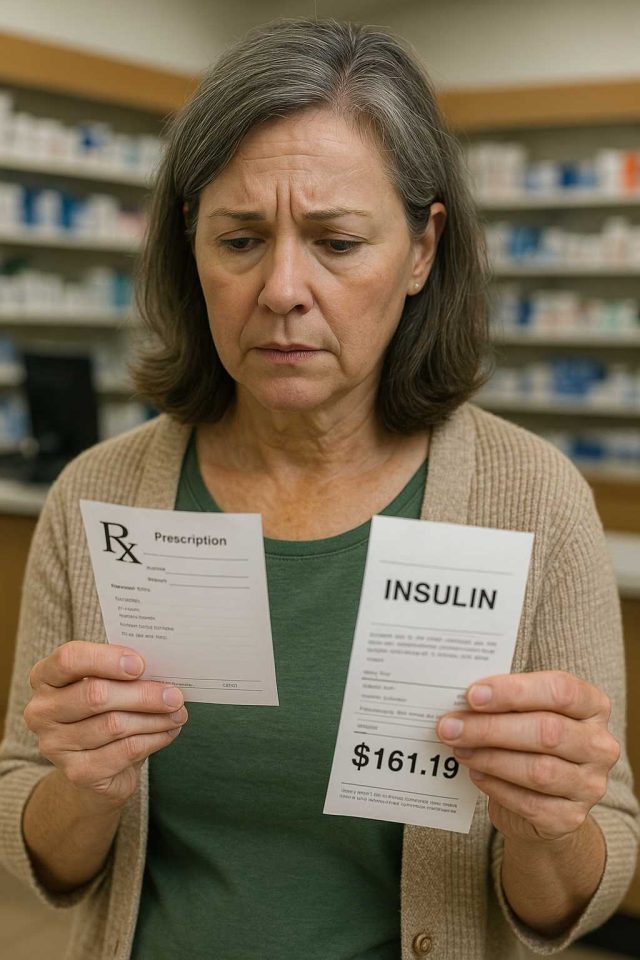
Imagine walking into a pharmacy on October 2 and finding that the cost of your essential medication has suddenly doubled. That scenario could become reality with the announcement of a 100% tariff on some imported drugs, effective October 1. For patients managing chronic conditions like diabetes, such changes could reshape access, affordability, and care in ways few anticipated. But what does this policy mean, and how might it affect both patients and providers?
Table of Contents
- Understanding the New Tariff on Imported Drugs
- Potential Impact on Patients and Providers
- Which Drugs Could Be Affected?
- Policy, Industry Response, and Patient Guidance
- Conclusion
- FAQs
Understanding the New Tariff on Imported Drugs
A 100% tariff essentially doubles the price of targeted products entering the United States. In this case, the focus is on specific imported drugs, many of which are critical for chronic disease management. The intent of the policy is to protect domestic manufacturing and reduce dependence on international supply chains. However, the immediate concern is affordability for patients.
For example, insulin analogs like Lantus and NovoLog, widely used in diabetes care, could be impacted if sourced or partially manufactured abroad. While generic options may remain unaffected, branded drugs produced overseas face sharp increases in cost. In contrast, domestically produced medications will likely become more competitive, but they cannot always meet demand in the short term.
Supporters of the tariff argue that it creates incentives for pharmaceutical companies to invest in U.S.-based production. Critics, however, warn that the move could limit patient access, especially for those already burdened by high out-of-pocket expenses. According to health economists, the long-term benefits of supply chain independence must be weighed against the immediate risk of reduced medication adherence.
For further context, related discussions have been covered in Diabetes in Control articles, which frequently highlight how policy changes ripple into patient care.
Potential Impact on Patients and Providers
The most direct consequence for patients is higher prices at the pharmacy counter. A doubling of cost may push some individuals to ration medications, a practice already observed among patients struggling with insulin affordability. Healthcare providers anticipate greater difficulty in ensuring adherence, especially for low-income or uninsured populations.
For clinicians, the challenge lies not only in prescribing but also in guiding patients through complex insurance and assistance programs. Physicians may increasingly consider switching patients from imported drugs to domestic alternatives, even if they are less familiar. Pharmacists, meanwhile, will face mounting pressure to identify affordable substitutions while counseling patients on new regimens.
In addition, this policy shift may place strain on insurance companies. Higher drug costs can lead to increased premiums, copays, or restrictions in formularies. As payers adapt, patients could see delayed coverage approvals or more frequent denials. While some patients may qualify for patient assistance programs, these often have strict eligibility requirements that exclude many middle-class families.
In contrast, domestic drug manufacturers may benefit in the short term. Their competitive advantage increases when foreign-made drugs double in price, creating new opportunities for expansion. Yet building capacity is not instantaneous, leaving a gap between policy implementation and market adaptation.
Which Drugs Could Be Affected?
Although the full list of affected products remains under review, several categories of imported drugs are at risk:
- Insulin analogs and injectables (Lantus, Humalog, NovoLog) when sourced abroad.
- Oral diabetes medications like sitagliptin (Januvia) and dapagliflozin (Farxiga) if imported.
- Blood pressure and cholesterol medications often prescribed alongside diabetes therapies.
The reach of the tariff may also extend beyond diabetes. Oncology treatments, antibiotics, and cardiovascular drugs represent other categories vulnerable to increased costs. Because supply chains are global, even medications finished in the U.S. may use imported components subject to tariffs.
For patients, this complexity makes it difficult to know which prescriptions will be affected until insurance companies and pharmacies adjust their pricing. Providers encourage patients to review their medication lists early and discuss potential alternatives with their healthcare team. For trustworthy health navigation resources, patients can consult Healthcare.pro.
Policy, Industry Response, and Patient Guidance
The healthcare industry is already responding with calls for clarity and relief measures. Advocacy groups argue that sudden spikes in drug prices disproportionately hurt vulnerable patients. They urge policymakers to consider exemptions for life-saving therapies. Pharmaceutical companies, on the other hand, are weighing whether to shift manufacturing bases or absorb some of the costs temporarily.
Providers and patient organizations recommend proactive strategies. Patients should check formularies, explore generic alternatives, and enroll in assistance programs before October 1. Physicians are advised to discuss cost implications with patients during routine visits. Pharmacists, too, are positioned to help by identifying substitutions or coordinating with prescribers on therapeutic alternatives.
For many, this change highlights the broader challenge of balancing healthcare economics with patient needs. While supply chain independence is an admirable goal, implementation without safeguards risks worsening existing disparities in care. Diabetes management already requires careful coordination; adding uncertainty in drug affordability may place unnecessary barriers on patients who are striving to control their disease.
To navigate these uncertainties, patients and providers alike can benefit from monitoring trusted sources such as the American Diabetes Association for policy updates.
Conclusion
The 100% tariff on some imported drugs beginning October 1 underscores the delicate balance between national policy and patient health. While the intention is to strengthen domestic manufacturing, the immediate effects could mean higher costs, reduced access, and greater challenges in diabetes care. For patients, the key takeaway is preparation: review medications, consult with providers, and explore assistance options. For providers, the emphasis must be on communication, education, and advocacy.
Ultimately, this policy shift may reshape the pharmaceutical landscape, but it also risks placing vulnerable patients in difficult positions. The coming months will reveal whether the long-term benefits outweigh the immediate costs.
FAQs
What is the 100% tariff on imported drugs?
It is a policy doubling the cost of selected foreign-made drugs entering the U.S., effective October 1.
Which medications could see price increases?
Insulin analogs, oral diabetes medications like Januvia, and other chronic disease therapies may be affected if imported.
How will this affect patients with diabetes?
Many patients may face higher out-of-pocket costs, potentially leading to medication rationing or changes in therapy.
Can insurance cover the price increase?
Insurance may absorb some costs, but patients could also see higher premiums, copays, or more restricted formularies.
What should patients do to prepare?
Patients should review their medications, consult providers about alternatives, and explore assistance programs before October 1.
Disclaimer
“This content is not medical advice. For any health issues, always consult a healthcare professional. In an emergency, call 911 or your local emergency services.”